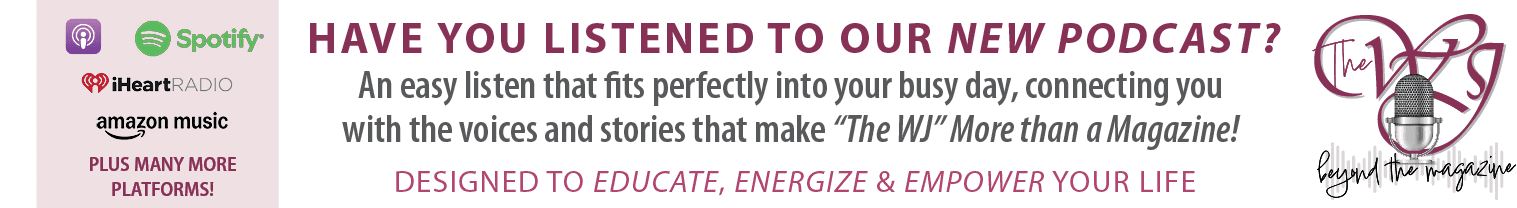
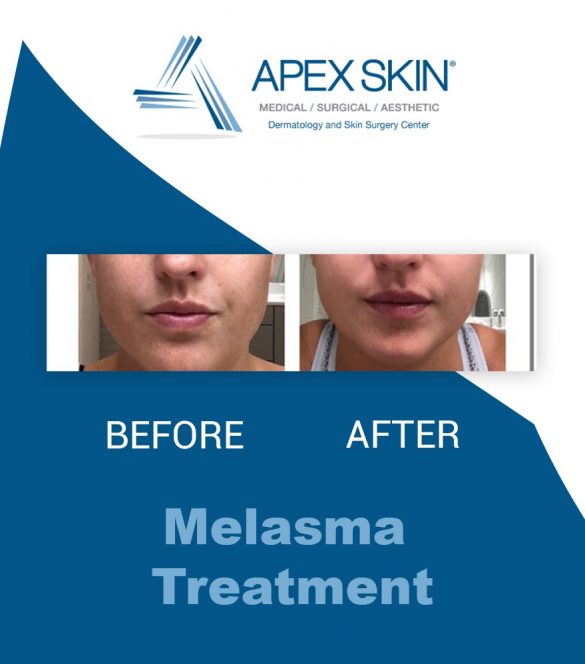
While melasma isn’t necessarily dangerous, it can still do some harm to our self-esteem, and it’s perfectly normal to want to do something about it.
Here to help us understand melasma so we can then treat it is Dr. Gregory R. Delost.
What is melasma?
“Melasma is a common, chronic, and recurring disorder of hyperpigmentation in which pigment producing cells known as melanocytes excessively deposit pigment in the epidermis and dermis.”
This presents as dark spots covering a single area, or the entire face.
It is often difficult to treat and therapeutically challenging leading to relapses and frustration. 
How does melasma affect patients?
Multiple studies have shown that melasma can be psychologically devastating.
“The majority of melasma patients report frustration, embarrassment, dissatisfaction with their appearance, strained interpersonal relationships, and depression.”
Once again, while melasma is essentially a “non-dangerous” skin condition physically, the emotional toll can lead to many negative experiences for patients.
How common is melasma?
Quite common. Melasma affects approximately 1% of the general population, but can be as high as 9-50% in high risk populations.
What are the causes of melasma?
There are several reasons why one would be plagued with melasma and unfortunately, some aren’t necessarily under your control.
Here are a few causes of melasma:
“Female gender, sun exposure, sensitivity to hormones, pregnancy, menopause, medications (such as oral contraceptive pills and hormonal replacement therapy), and genetics.”
How is melasma diagnosed?
Melasma is typically diagnosed based on clinical presentation.
“The lesions are usually symmetric and common sites include forehead, cheeks, nose, upper lip, chin, and jawline.”
Sometimes, a skin biopsy can be helpful to determine the depth of the melanin to subsequently help guide treatment.
What is the typical clinical course of melasma?
Melasma tends to be chronic and recurrent. However, sometimes pregnancy-related melasma can go into spontaneous remission.
Unfortunately, sometimes it can persist for months, years, and even indefinitely. Even after successful treatment, melasma can relapse with even mild sun exposure.
This makes it a difficult and sometimes downright annoying skin condition to treat, but there are treatment options available to manage it.
How do you treat melasma?
Every patient is different, and therefore requires a unique and tailored approach.
“In most cases, a multimodality approach is required, incorporating photoprotection, skin lighteners, exfoliants, antioxidants, and resurfacing procedures, based on the patient’s characteristics and clinical presentation.”
Ultimately, only a dermatologist can help you treat this skin condition, because it depends on the severity and cause.
What type of photoprotection is needed?
Strict photoprotection, including sun avoidance, sun-protective clothing, and broad-spectrum and visible light sunscreens, is an essential component of all treatment and prevention regimens for melasma.
“Daily, patients should use a broad-spectrum sunscreen with a sun protection factor (SPF) of 50 or higher.”
Sunscreen should be applied in an adequate amount in the morning and reapplied every two to three hours while outdoors.
How to prevent melasma?
Topical skin-lightening agents are the first-line therapy for melasma and include hydroquinone and/or non-hydroquinone skin lighteners, such as azelaic acid, kojic acid, or niacinamide.
“For patients with moderate to severe melasma, the fluocinolone, hydroquinone, and tretinoin triple combination cream (TCC) is preferred.”
Ultimately, your best line of defense will be adequate skin protection.
What are some other treatments for melasma?
Chemical peels, oral tranexamic acid, lasers, and light treatments can also have an impact on keeping recurring and stubborn melasma at bay.
You can book an appointment with a dermatologist if you’d like to explore these options.
What about maintenance therapy?
Routine approaches for prevention of relapse involve the aggressive use of broad-spectrum and visible light sunscreens as well as maintenance treatment with non-hydroquinone lighteners, such as azelaic acid, kojic acid, niacinamide, and retinoids.
While melasma can be stubborn and difficult to deal with, you do have options for preventing and treating its appearance. Make sure to meet with a qualified dermatologist in order to understand exactly what we can do to help you.